What is Diabetic Retinopathy ?
An increasing incidence of diabetes mellitus poses a major health problem in India. The contributing factors are:
- an inappropriate diet, high intake of fat and carbohydrates
- sedentary lifestyle
Diabetes may affect both the young (type I) and the old (type II). The latter type is far more common.
Regardless of the type of diabetes, many diabetic patients develop a complication called diabetic retinopathy, a change in the retinal blood vessels that leads to loss of vision.
How does diabetes affect the eye?
Diabetes causes weakening of the walls of the blood vessels in the body. The tiny, delicate retinal blood vessels are particularly susceptible. This deterioration of retinal blood vessels, accompanied by structural changes in the retina, is termed diabetic retinopathy and leads to loss of vision.
Diabetic retinopathy is gradual in onset and is related to the duration of diabetes. High blood glucose levels, high blood pressure and genetics influence the development and progression of diabetic retinopathy
What are the stages of Diabetic Retinopathy?
There are two main stages of Diabetic Retinopathy:
Non-proliferative Diabetic Retinopathy (NPDR): In this stage you may not have much of visual symptoms, but the retinal findings can be noted only by your ophthalmologist after dilated fundus examination. The leaky blood vessels in Diabetic Retinopathy lead to leakage of fluid (retinal edema), leakage of blood (retinal hemorrhages), and small out-pouching of the retinal blood vessels (micro-aneurysms). NPDR is further sub divided into 4 stages depending on the clinical findings.
- Retinal edema in the central area is called as diabetic macular edema (DME) may occur, thereby reducing vision.
- These changes in the retinal blood vessels can also lead to their blockage and retinal ischemia, which is also a cause for decreased vision.


Proliferative Diabetic Retinopathy (PDR): This is the next stage of Diabetic Retinopathy wherein new, weak blood vessels grow or proliferate at the back of the eye. These weak new blood vessels may bleed into the vitreous cavity and cause severe visual loss.
What are the symptoms of Diabetic Retinopathy?
In the early stages, you may not have any symptoms. However, as the Diabetic Retinopathy progresses, you may perceive the following symptoms:
- Blurred vision
- Darkened or distorted images (commonly noticed in DME)
- Dark / Black spots (floaters) in vision
- Total loss of vision
What are the risk factors of Diabetic Retinopathy?
Anyone with Type 1 or Type 2 Diabetes is at risk for Diabetic Retinopathy.
You are at a higher risk if you have:
- Uncontrolled and high blood sugar
- Number of years of diabetes
- Uncontrolled blood pressure (uncontrolled hypertension)
- Increased cholesterol
- Kidney disease (Diabetic Nephropathy)
- Pregnancy
In some cases, people with good blood sugar, blood pressure, and cholesterol may still develop Diabetic Retinopathy. To be safe, all diabetics should regularly see an eye doctor for screening.
How is Diabetic Retinopathy diagnosed?
Diabetic Retinopathy can take years to cause blindness. In the early stages, it is treatable. If you are a diabetic, visit your eye doctor every year. Early detection is very important and can save your eyesight.
- Every eye examination the following tests would be adviced by your doctor
- Visual aquity testing (distance and near)
- Detailed eye examination (slit lamp biomicroscopy)
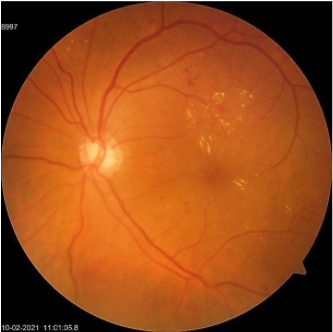
- Dialated fundus examination (ophthalmoscopy / fundoscopy)
- Depending on your retinal findings, the doctor may advice for some special tests:
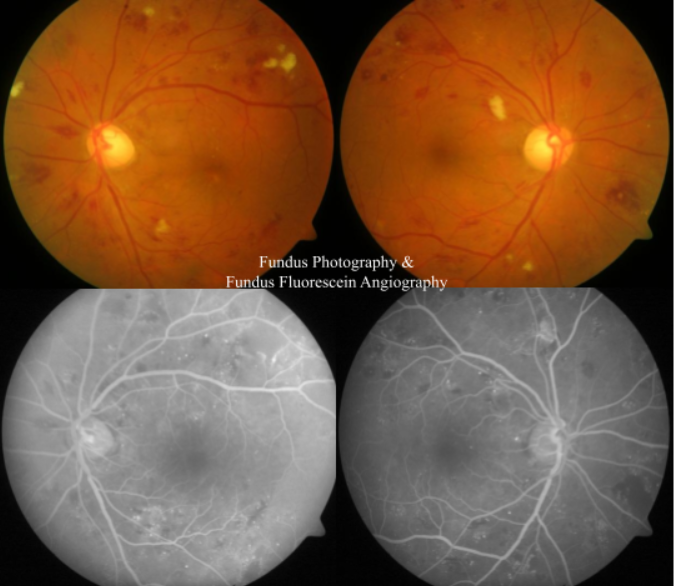
- Fundus photography
- Fundus Flurescein Angiography (FFA)
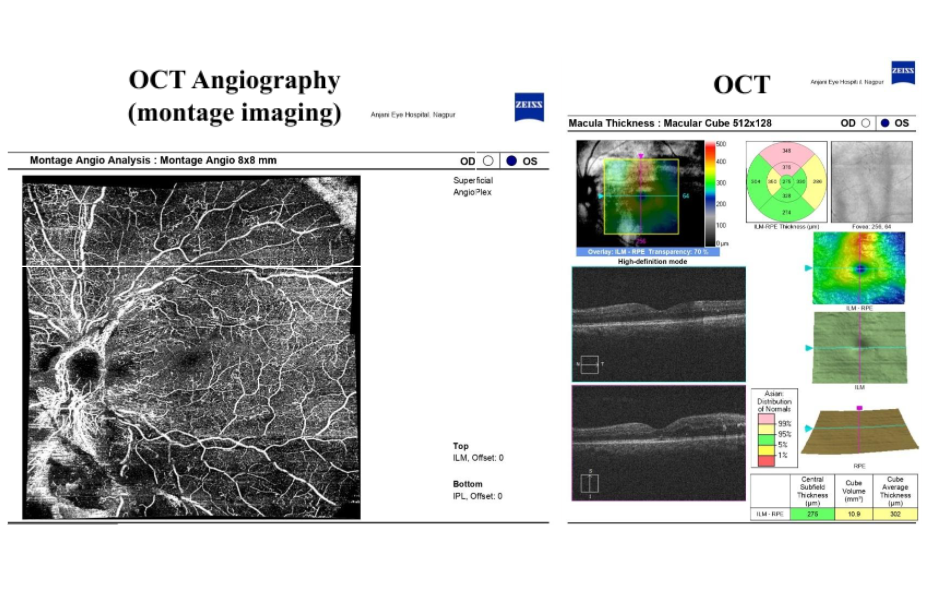
- Optical coherence tomography (OCT)
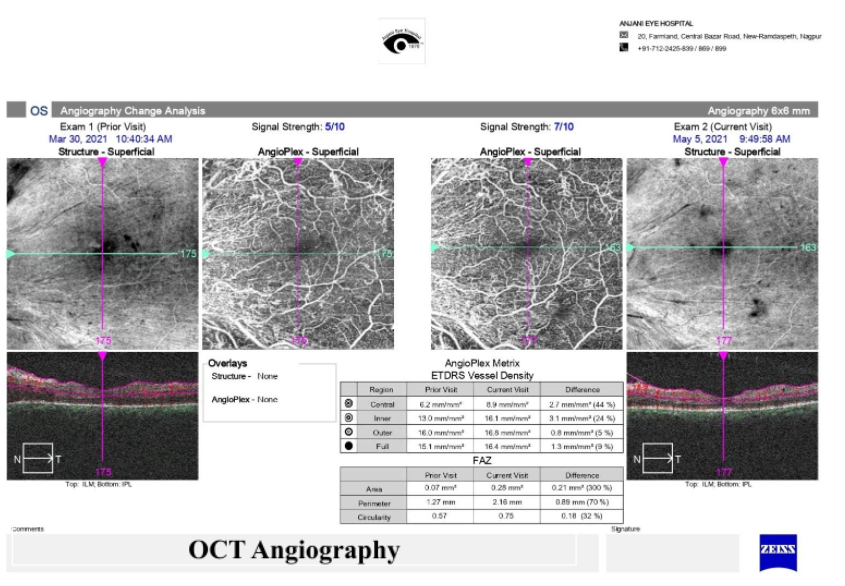
- OCT Angiography (OCT – A)
Your eye doctor would decide on the stage of Diabetic Retuinopathy in your eye, based on these tests. He / She would then plan on further management in the form of observation or treatment.
Anjani Eye Hospital, is equipped with top of the class equipment (FFA & OCT-A) from Carl Zeiss, Germany in the diagnosis and treatment of Diabetic Retinopathy.
What are the treatment options of Diabetic Retinopathy?
Depending on the stage of Diabetic Retinopathy your eye doctor would suggest various treatment options:
Observation – If your doctor feels that your Diabetic Retinopathy does not require any treatment as of now, he / she may advise you for periodic followup visits (ranging from 3 monthly to yearly reviews).
Retinal Lasers (laser photocoagulation) – Laser photocoagulation for Diabetic Retinopathy is used to prevemt further loss of vision and not to restore lost vision. It can be used in 2 scenarios for traetment of Diabetic Retinopathy.
- Diabetic Macular Edema (DME) – Laser is used here to reduce the swelling in the retina by treating the leaky blood vessels (microaneurysms). However, laser is used lesser now a days for this indication with the routine use of intravitreal injections.
- Proliferative Diabetic Retinopathy (PDR) – Pan Retinal Photocoagulation (PRP) also called as scatter laser treatment is used in PDR to reduce the possibility of retinal ischemia and in turn reduce the formation / regress the new retinal vessels. This laser is done in multiple sittings (commonly 3sittings).

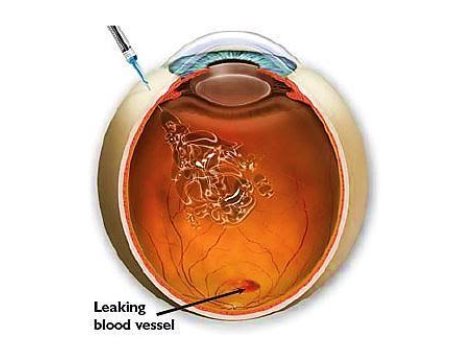
Intravitreal Injections – In Diabetic Retinopathy these are used to prevemt further loss of vision and not to restore lost vision. The commonly used injections in Diabetic Retinopathy treatment are:
- Anti Vasculo– Endothelial Growth Factors (Anti-VEGF)– These are used commonly for treatment of DME (may need 5-6 injections), fresh vitreous hemorrhage (bleeding in the eye), or pre-operatively (before vitectomy surgery). The various Anti-VEGF injections available are Lucentis / Accentrix, Eylea, Razumab and Avastin.
- Steroids – These are used for the treatment of DME. The commonly used intravitreal steroids are Ozurdex (dexamethasone) or Triamcinolone Acetonide (TA).
Vitrectomy Surgery – In some eyes with PDR, laser treatment or intra-vitreal anti-vegf would not be able to restore or save vision. In such eyes the eye doctor would suggest vitrectomy surgery to clear the blood in the eye. He / she would also treat the underlying cause of the bleeding (new vessels) and additionally laser the retina.

Eye examination in diabetic retinopathy: Every diabetic is a potential candidate for diabetic retinopathy. There are no symptoms at the initial stages. Periodic eye examination with dilated pupils is the only way to detect early disease and prevent further deterioration of vision.
Frequently Asked Questions (FAQ)
Controlling your blood sugar can prevent further damage to the retina. But, it most likely will not reverse the damage that has already occurred. You will need to be treated to stop the retina damage from progressing. This damage is linked to how well your diabetes is controlled. So, while controlling your blood sugar may not be a cure, it can help slow the disease.
Strict blood sugar control is a must, but it may not be enough. For this reason, all diabetics should get an eye screening every year.
Retinal changes are the major problem, but at times diabetes can also cause a rise in eye pressure (glaucoma), clouding of the lens (cataract), and weakness of the optic nerve or eye muscle. Cataracts often occur at a younger age in diabetic patients. Glaucoma can cause damage to the optic nerve. In fact diabetes is one of the several possible causes of glaucoma.
Damage to the small vessels of the optic nerve can affect vision, and weakness of the eye muscles may cause double vision. A diabetic is also more likely to develop sudden vision loss due to occlusion of the retinal vessels (branch or central retinal vein occlusion), bleeding in the vitreous cavity, detachment of the retina, or infections of the cornea and vitreous.
Diabetic Retinopathy can be prevented by controlling your diabetes. You must also control your blood pressure and cholesterol levels. Regular checkups with your primary care physician and an eye doctor are necessary for prevention.
The best way to control a diabetic eye disease is to find and treat it early. Even if you control your diabetes, your eyes are still at risk. The ONLY way to protect your vision is by getting your eyes checked every year.
Yes. This is actually an important sign of Diabetic Retinopathy. In early stages, there is very little bleeding. But in the later stages, new fragile blood vessels grow in the retina. These vessels are so weak that blood may bleed out of the blood vessels into the surrounding fluid. This can cause cloudy vision.
If you have diabetes, your body does not use and store sugar properly. This can damage the small blood vessels in the retina. The retina is the light-sensitive tissue that helps detect images and send them to the brain. So, when it is damaged, vision is greatly affected.
Vitrectomy surgery for Diabetic Retinopathy is usually done to safe guard your vision. If the central area of the retina is damaged or if the detachment is treated at a later stage, complete visual recovery cannot be guaranteed. But, there is a chance that your vision will not deteriorate.
Silicon oil inside the eye is usually well tolerated. However, few patients might experience raised intraocular pressure, or double vision. These side-effects usually improve after the oil is removed (3-4 months after surgery).
If silicon oil is left in the eye, there is a high chance that cataract would set in, the eye pressure may increase, causing nerve damage and eye pain.
The decision regarding usage of gas or silicon oil inside the eye is usually taken by the operating surgeon based on the condition of your eye during surgery. It is better to use the filling that is best for your eye health than to try and avoid another surgery.
If you choose not to get the vitrectomy surgery done, your retinal condition may worsen due to progression of Diabetic Retinopathy. You may lose your vision completely as the retina becomes more damaged. You can also develop cataract. If you have uveitis or glaucoma, you may experience eye pain. In the long run, your eyes might even shrink.
Surgery offers a chance to save your sight, and sometimes improve it as well.
At Anjani Eye Hospital vitrectomy surgery for Diabetic Retinopathy is done as day care procedure and most of the patients opt to go home the same day. However, you would need a follow-up visit the next day stay.
You would have to maintain the position as explained to you for a minimum of 5-10 days.
Laser treatment for Diabetic Retinopathy will prevent the progression of the disease. In some cases, vision may improve slightly. Typically, vision that is lost to Diabetic Retinopathy cannot be restored. So, the longer the treatment is delayed, the higher the chance of permanent loss of vision.
This depends on your eye’s response to the first laser treatment. Your doctor will decide if it is needed. Unfortunately, if the retinal problem recurs, then another round of laser treatment may be required.
Laser treatment is a very safe procedure. Both the side effects and the possible complications are extremely rare. The benefits of laser treatment in Diabetic Retinopathy far outweigh these rare complications.
Yes, you can perform all your daily activities as you normally do after laser treatment for Diabetic Retinopathy.
Generally, a few patients may experience mild pain or heaviness in the eye, but these last for about 3-4 hours. These patients may use eye drops to reduce the pain.
You need to have a regular check-up with your eye doctor as per the condition of your Diabetic Retinopathy. This will allow doctors to see how well the treatment is working. It can also help them see if any new retinal damage has occurred.
Intravitreal injections are used to treat many diseases that cause irreversible vision loss. They mainly work by preventing further damage. Your vision may improve slightly in some cases, but there is no guarantee.
Treatment with intra-vitreal injection varies for different retinal conditions. For Diabetic Retinopathy (diabetic macular edema) the protocol followed at Anjani Eye Hospital is evidence based with eyes needing one injection per month for about 5-6 months. This depends on your response to the injection treatment as well.
Intravitreal injections are given through the white portion of the eye. You will be given anesthetic eye drops, so you should not feel any pain and the injection should not cause any problems.
There are a few, but they are very rare. Injection treatment is a relatively safe procedure. In fact, you can go home the same day as the treatment.