What is Uveitis?
Uveitis is an inflammation that occurs in the middle pigmented layer (uvea) of the eyeball, which lies between the retina (on the inside) and sclera and cornea (on the outside). It can also lead to inflammation in the adjacent areas, like the retina and fluid in the back of the eye (called vitreous). When the uvea is inflamed, you may get eye pain, eye redness and blurred vision. Uveitis can lead to permanent vision loss and hence should be treated at the earliest.
What causes Uveitis?
While the basic cause for Uveitis remains undetermined, it may be a manifestation of systemic diseases. Broadly, the causes of Uveitis could be divided into:
- Infective
- Bacterial (Tuberculosis, Leprosy, Syphilis etc…)
- Viral (CMV, Herpes etc…)
- Parasites (Toxoplasmosis, hydatid etc…)
- Fungal
- Auto-Immune (arthritis related, psoriasis related etc…)
- Post eye injury
Doctors often call for laboratory tests, X-rays and consultations with specialists to determine the cause of Uveitis. However, even after detailed investigations, the exact cause of Uveitis may not be found.
What are the types of Uveitis?
Uveitis can be of four types, depending upon the location of the inflammation.
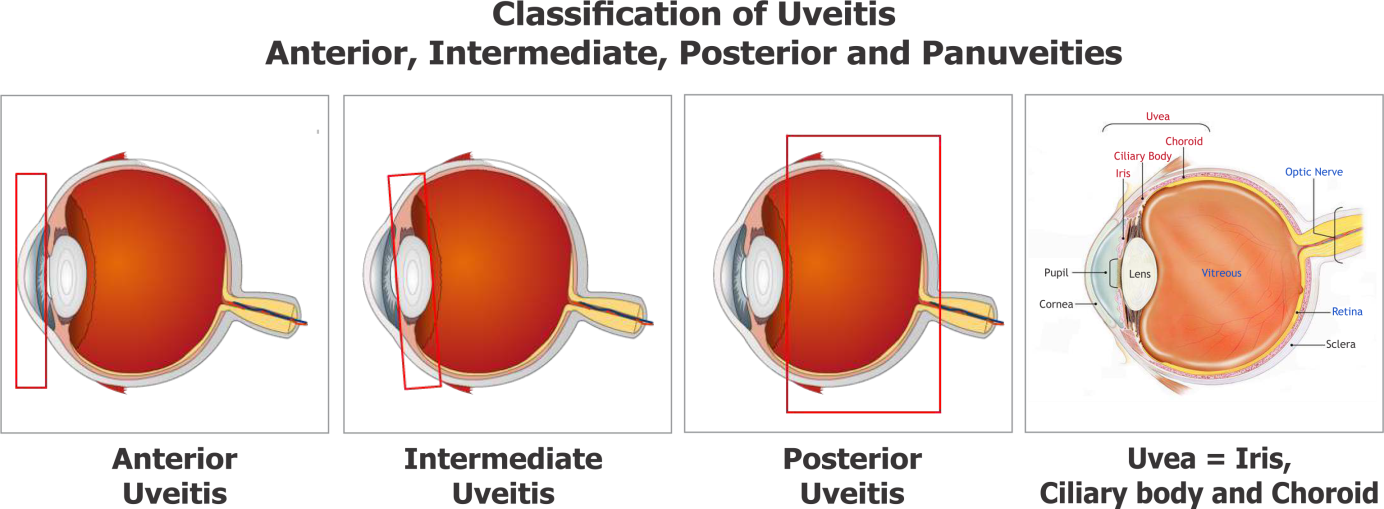
1. Anterior Uveitis
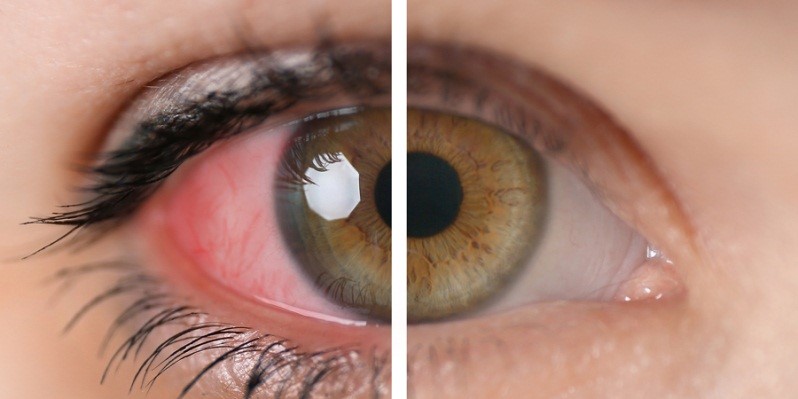
This kind of Uveitis affects the front or anterior portion of the eye. The common symptoms are redness, watering, decreased vision, pain in the eye and photophobia (intense discomfort while looking at light). In low-grade inflammation, the eye may appear normal but still have signs of damage.
2. Intermediate Uveitis
Also known as par planitis, consists of vitritis – inflammation in the vitreous. The patient usually sees black spots in front of the eye. There may be loss of vision due to fluid accumulation in the central area of the retina.

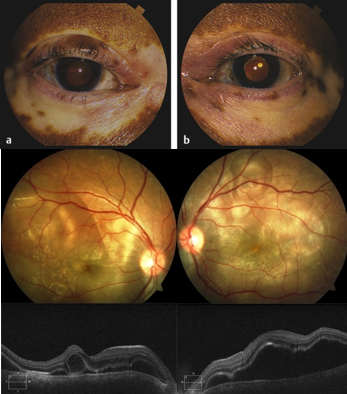
3. Posterior Uveitis
This type affects the back or the posterior portion of the eye. The eye may appear normal or there may be little inflammation in the front. The inflammation may affect the retina, posterior choroid or both. The inflammation may be localized to a particular area or widely spread. Patients usually complain of black spots in vision, poor vision, or the absence of central or peripheral vision.
4. Panuveitis
Panuveitis affects the entire uveal tract (from the front to the back). It often causes a distinct blurring of the vision with varying degrees of pain and redness. This is also associated with inflammation in the vitreous cavity at the back of the eye causing the patient to perceive black spots in vision.
What is the treatment for Uveitis?
The goal of the treatment for uveitis is to: relieve pain, reduce and / or stop vision loss, and treat the systemic disease or infection. Even though there may not be a permanent cure for Uveitis, each attack can be treated, depending upon the cause, severity and location of the inflammation. The treatment may include eye drops, injections under the eye or oral medication.
The most commonly prescribed eye drops relieve the muscles inside the eye and help to dilate the pupil, temporarily paralyzing the sphincter muscles, to relieve the pain. This may cause some difficulty in near vision and increase the feeling of glare in bright light. Patients are advised to use dark glasses while going out in the day.
To control inflammation, steroids may be given in the form of drops, injections around the eye or tablets. Sometimes, a depot steroid injection may be used, which causes a slow release of the drug into the eye. The drug usually lasts for several weeks.
When the inflammation is extensive or severe, oral drugs such as steroids and immunosuppressive drugs are needed. These drugs have potential side effects, but they are often not serious and their effects are reversible, once treatment is discontinued.
What are the precautions to be taken during treatment of Uveitis?
- Please take the medicines as advised by the doctor; do not start or stop the medication on your own. If you are on oral steroid therapy and have to undergo any surgery, please inform your doctor. If you have taken oral steroids for more than two weeks, do not stop suddenly, as this could have serious problems.
- Keep your medication where you can see it easily.
- Schedule your medication intake around your daily routine, like when you wake up in the morning, at meal times or at bedtime.
- If you forget to use your eye drops, use them as soon as you remember, instead of waiting till the next scheduled time. Then get back on schedule for the next dose.
- Watch out for side effects like changes in vision. Inform your doctor immediately about them or on your next appointment. Schedule your check-ups regularly.
- When consulting doctors for other problems, tell them about the medicines that you are using. Eye medications can affect other parts of the body too.
What are the potential side effects of the medications used for Uveitis?
- Oral steroids may cause acidity, mild stomach pain, increase in weight, acne or pimples. In rare cases, they can induce diabetes, hypertension, osteoporosis (weakening of the bones), nervousness and depression.
- Women are advised to avoid pregnancy (contraceptive devices can be used) while on treatment with oral steroids or immunosuppressive drugs.
- Some immunosuppressive drugs interfere with the basic metabolic process of the body; many of them cause bone marrow depression, thereby reducing the blood count. Patients are advised periodic blood tests while taking the treatment, to monitor the side effects of the drugs.
- Sometimes some antibiotics (anti tubercular medications) may be started by your doctor. These medications may lead to decreased vision (sudden or delayed). These medications are also known to cause abnormalities in liver function. Your doctor may therefore advice periodical eye checkups and blood tests to monitor these side effects. In the rare instance of occurrence of these side effects, you need to report immediately to your doctor or if noted by your doctor at the regular follow-up visit, he / she may change the medications and these side effects could be completely reversed.
Frequently Asked Questions (FAQ)
Yes, in many cases Uveitis can recur. The frequency and severity of the attacks is however, unpredictable. Consult your ophthalmologist as soon as you notice any signs of recurrence; this will make the treatment simpler and lead to a quicker resolution of Uveitis.
Patients with Uveitis can develop complications like cataract, glaucoma (raised eye pressure) and macular edema (fluid accumulation in the central part of the retina). Such complications can be managed medically or surgically once the inflammation is controlled. However if these complications are left untreated they can lead to permanent loss of vision.
Uveitis can lead to loss of vision if not managed properly. However, with modern diagnostic methods, better medication and surgical techniques, the prognosis for most patients is very good. It is critical that the disease is identified early and treated properly. It is also important for Uveitis patients to get their eyes checked periodically, even if there are no symptoms.
You must realize that every case of Uveitis is different – your case may not be exactly like any of the types described here. Do not hesitate to ask your doctor for further information to the treating doctor.

