What is Glaucoma ?
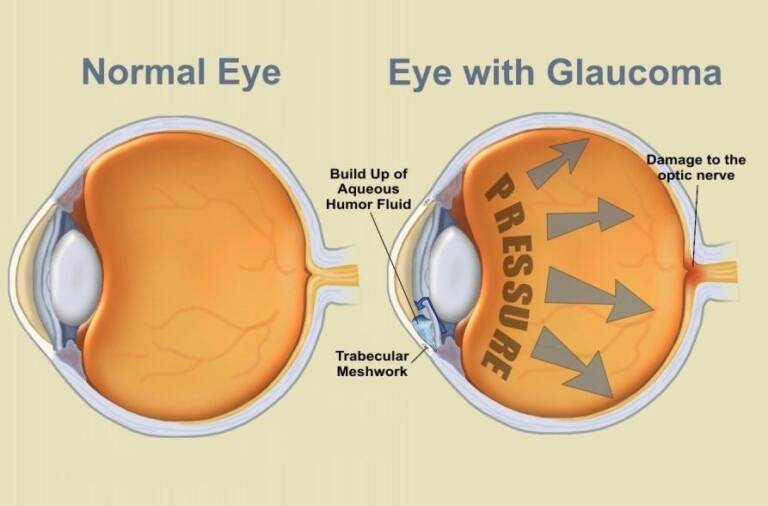
Glaucoma is a group of disorders in which the pressure of fluid within the eye gradually increases to a level that irreversibly damages the sensitive tissues of the eye, most notably the optic nerve which transmits visual images to the brain. It is the second most common cause for blindness. Though there is no cure for this condition, doctors can help preserve vision for the patient.
What are the causes of Glaucoma?
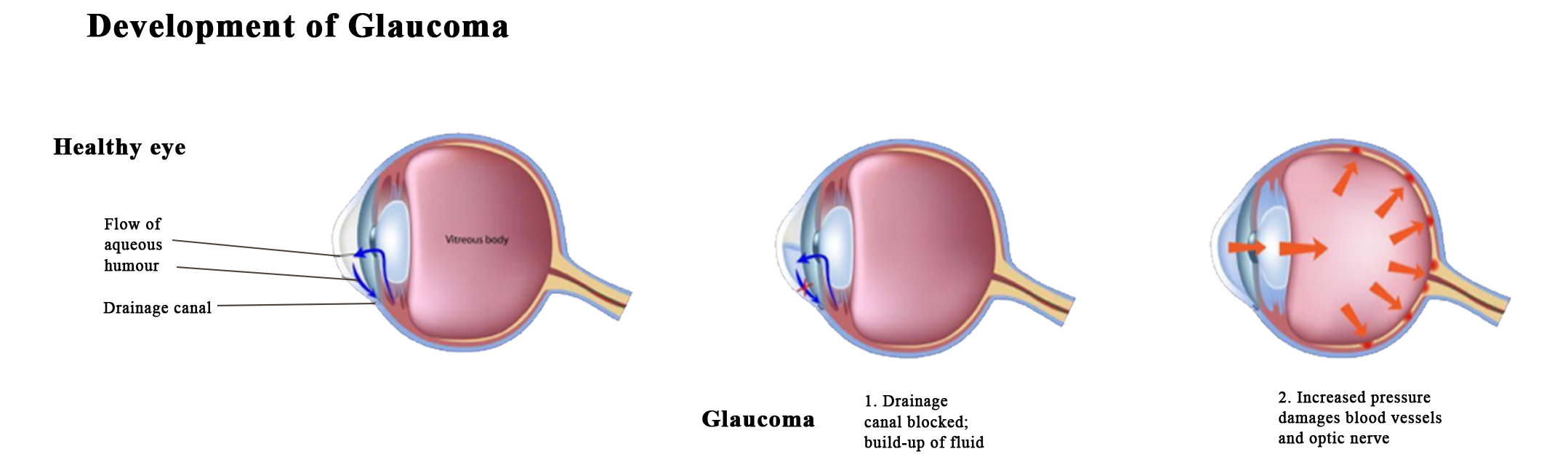
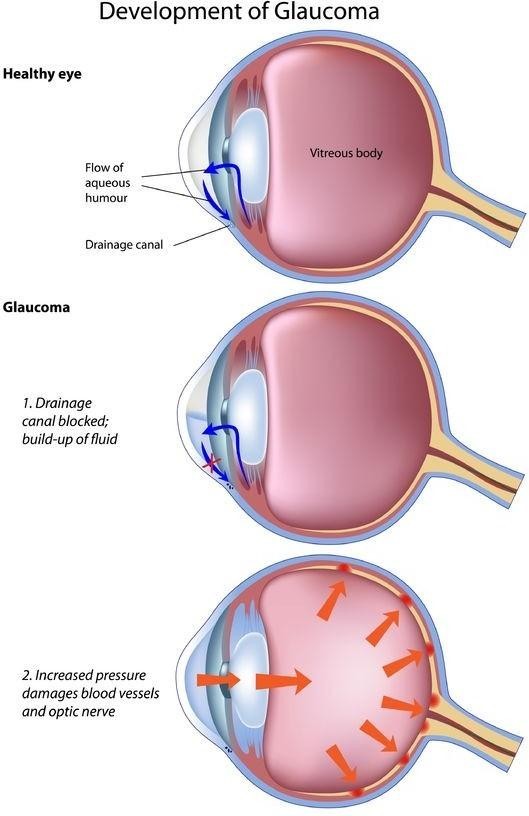
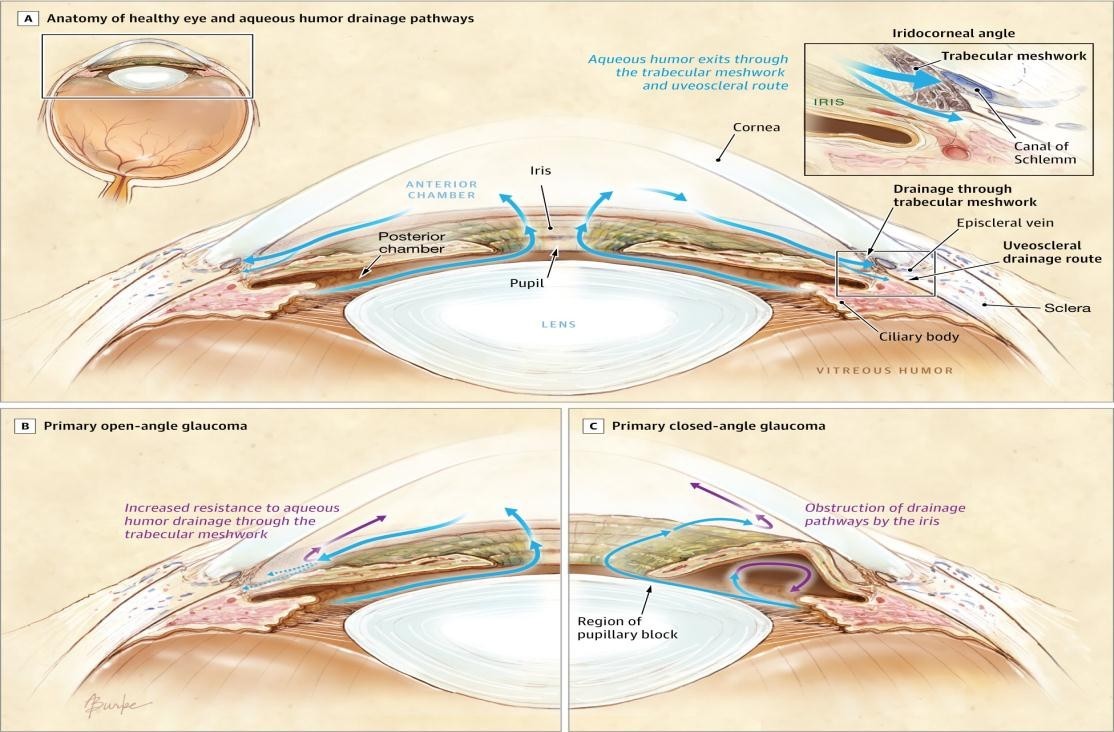
Front part of the eye, the anterior chamber, is filled with fluid (aqueous humor). Normally, the fluid drains out of the eye through a sieve (trabecular meshwork) located in the angle of the anterior chamber (the internal junction between the iris and the cornea). If the drainage of this fluid from the anterior chamber is restricted, pressure builds up within the eye causing irreversible damage to the optic nerve thereby causing a permanent loss of vision.
- Glaucoma can sometimes occur with a statistically “normal” IOP. Hence the vulnerability of the optic disc is another factor that needs to be considered. Accordingly, the diagnosis of glaucoma requires more than just the mere measurement of intraocular pressure.
- Individuals over the age of 40 as well as persons with myopia, diabetes or a family history of glaucoma are at an increased risk of developing glaucoma.
- Individuals who have sustained injury to the eye or who are using corticosteroids are at an increased risk.
-
Glaucoma can sometimes occur with a statistically "normal" IOP. Hence the vulnerability of the optic disc is another factor that needs to be considered. Accordingly, the diagnosis of glaucoma requires more than just the mere measurement of intraocular pressure.
-
Individuals over the age of 40 as well as persons with myopia, diabetes or a family history of glaucoma are at an increased risk of developing glaucoma.
-
Individuals who have sustained injury to the eye or who are using corticosteroids are at an increased risk.
What are the types of Glaucoma?
There are several types of glaucoma all of which show an increased IOP and show damages on the optic nerve.
Open angle glaucoma: There is an increase in resistance to the outflow in the drainage channel (trabecular meshwork) which causes a rise in the IOP. This type develops gradually and patient may have a loss of peripheral vision, leaving only central or ‘tunnel’ vision. This occurs more amongst people above 45 years of age.
Angle closure glaucoma: There is a relative block to the flow of fluid by the iris blocking the drainage channel in the angle, which causes raised pressure. Stress, anxiety, and reading may also precipitate an attack, which may resolve on its own, but recur after some time.
Developmental glaucoma: which may be further divided into:
- congenital glaucoma in infants from the time of birth) and
- juvenile glaucoma (occurs in children and young adults).
Secondary Glaucoma: Occurs due to other causes such as the use of steroid drops without prescription, following trauma (injury) to the eye, or sometimes due to some conditions inside the eye (neovascular glaucoma due to venous occlusions)

What are the symptoms of Glaucoma?
- Most types of glaucoma remain asymptomatic until advanced stage and that is why glaucoma is termed as the “silent thief of sight”. Hence periodical checkup, especially for those at risk, is necessary to detect glaucoma early.
- Some individuals, especially if there is a rapid buildup of eye pressure, may experience one or more of the following symptoms:
- Pain around the eyes when coming out from darkness (e.g., as soon as the person comes out of a theatre).
- Coloured rings (halo) seen around bulbs, especially during mornings and nights.
- Frequent change of reading glasses, headaches, pain and redness of the eyes.
- Reduced vision in dim illumination and during nights.
- Gradual decrease of side vision.
- Blurring of vision.
How is Glaucoma diagnosed?
The treatment for the different types of glaucoma varies, hence it is necessary for your doctor to diagnose the right type of glaucoma by conducting tests on your eye.
- Detailed examination of the eye on slit lamp biomicroscope, which is done on a routine basis.
- Eye pressure measurement with an applanation tonometer (mounted on the slit lamp), after instilling anaesthetic eye drops in your eyes.
- Examination of the angle of the anterior chamber – “gonioscopy” to determine the type (open angle / closed angle) of glaucoma. This is performed by using a specialised lens placed on the cornea of the eye after instilling anaesthetic eye drops in your eyes.
- Inspection of the optic nerve and the central retina by Ophthalmoscope or Slit lamp after dilating your pupil.
- Testing the peripheral vision by a computer assisted test called “automated perimetry” (visual field examination).
- If available, optical coherence tomography (OCT) to assess changes in the retinal thickness and optic nerve head.
-
Detailed examination of the eye on slit lamp biomicroscope, which is done on a routine basis.
-
Eye pressure measurement with an applanation tonometer (mounted on the slit lamp), after instilling anaesthetic eye drops in your eyes.
-
Examination of the angle of the anterior chamber - “gonioscopy” to determine the type (open angle / closed angle) of glaucoma. This is performed by using a specialised lens placed on the cornea of the eye after instilling anaesthetic eye drops in your eyes.
-
Inspection of the optic nerve and the central retina by Ophthalmoscope or Slit lamp after dilating your pupil.
-
Testing the peripheral vision by a computer assisted test called “automated perimetry” (visual field examination).
-
If available, optical coherence tomography (OCT) to assess changes in the retinal thickness and optic nerve head.
Baseline tests are necessary for future comparison and periodic examinations are essential to check the progression of the disease.
What is the treatment for Glaucoma?
- Glaucoma cannot be cured and any loss of optic nerve function in the form of loss of vision and loss of visual fields cannot be recovered. Appropriate treatment and regular follow-up can preserve residual vision from further damage.
- Treatment of glaucoma has to be individualized as per the eye and the severity of the condition for that eye.
- Medical management in the form of eye drops are available
- to reduce fluid formation within the eye or promote their drainage from the eye. For most glaucoma patients, regular use of medications will suffice to control the pressure inside the eye.
- to open up the angle of the anterior chamber and thus improve outflow.
- Laser treatment to make a hole in the iris (iridotomy) works great in early stages of angle closure glaucoma but not in advanced stages where medications and surgery remain the mainline of treatment.
- Laser treatment to the trabecular meshwork (Laser trabeculoplasty) is done in few cases with open angle glaucoma. However, this procedure may need to be repeated at a later date if the IOP increases again.
- Surgical management is either trabeculectomy (done frequently if your eye pressure is not controlled with eye drops) or shunt procedures in eyes with refractory types of glaucomas.
- Cyclocryo or Cyclophotocoagulation are procedures done in eyes which have gone blind due to advanced glaucoma.
- Medical management in the form of eye drops are available
Remember
- Glaucoma cannot be cured, only controlled.
- Vision lost due to glaucoma cannot be recovered.
- Early detection and treatment of glaucoma, before it causes significant visual loss, is the ideal way to control the disease.
- It is essential that persons above the age of 40 have their eyes examined periodically to detect glaucoma early.
- Glaucoma is not an infectious disease, but may be hereditary. So, if anyone in the family has glaucoma, it is advisable that the rest of the family members have their eyes examined, periodically.
- Once diagnosed as having glaucoma, the patient should be committed for lifelong treatment and periodic eye check-up.
- Drugs prescribed should be regularly used at specified time, to ensure round-the-clock pressure control. Medications may cause a few undesired effects. In the event of any adverse effect, the patient must approach the ophthalmologist immediately for alternate treatment.
- Glaucoma is a potentially blinding condition and the need for life long monitoring is essential.

