What is Keratoconus ?
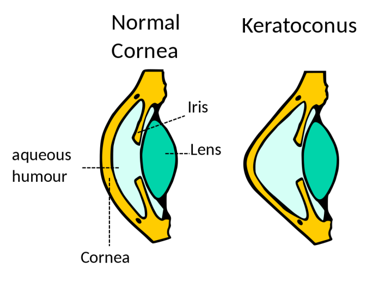
Keratoconus is when the cornea of the eye bulges out in the shape of a cone. This happens when the front layer of the eye (the cornea) starts to thin. At first, the bulge may be mild but the condition can get worse over time. It normally affects both eyes.

What are the causes of Keratoconus?
The cause of keratoconus is not known.
Risk Factors:
- Family history of keratoconus
- Environmental factors – frequent eye allergies and rubbing your eyes
- Conditions like retinitis pigmentosa, Down syndrome, hay fever, and asthma
- Hormonal factors
Keratoconus affects about 1 in every 2000 Indians. It is most common in teenagers and young adults in their mid-teens and 20s.
What are the symptoms of Keratoconus?
- Blurry vision
- More sensitive to light and glare
- Frequent changes in spectacle power
- Sudden cloudy vision accompanied by sudden onset of pain
How is the Keratoconus diagnosed?
The eye doctor will do refraction to check the eye power and visual acuity of your eye and a detailed eye examination. He / she would do a detailed eye examination with slit lamp and dilated retinal examination.
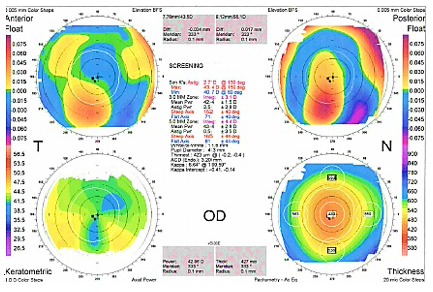
One sign of the disease is a bulging cornea. The eye doctor can notice this bulge on clinical eye examination. He / She may notice change in your eye power change (spherical and astigmatic). Other findings noticed by your doctor on examination are scissor reflex on retinoscopy and high keratometry values suggestive of irregular astigmatism. He / She may then advice for some special tests, corneal topography (test for measuring the contour / curvature of the cornea) and corneal pachymetry (test for measuring the thickness of the cornea). These special tests are useful to monitor the progression of Keratoconus (therefore, your doctor might advise these tests every 6 months)

What are the treatment options for Keratoconus?
The treatment of Keratoconus depends on the stage of the disease and condition of the cornea. The management of Keratoconus can be broadly divided into medical and surgical.
Medical
- Treatment of ocular allergies (with steroids and other anti-allergic eye drops),
if any, should be done in addition to spectacles and contact lenses. - Spectacles / Contact lenses
- In the early stages, vision can be corrected with spectacles.
- In later stages, individually-fitted contact lenses (hybrid lenses, scleral lenses, piggyback lenses) can be used. This lens gives better vision. However, it can also increase your sensitivity to light and glare. Finding a comfortable lens can be difficult, but it is important that the lens fits well. Poorly fitting lenses can damage the cornea even more.


- If you cannot wear contact lenses, or have corneal scarring, or if your Keratoconus is progressing (as per the test results), your doctor may suggest surgical interventions.
- C3R (corneal collagen crosslinking)
- Corneal Transplant (penetrating keratoplasty / deep anterior lamellar keratoplasty)
- Corneal Ring Implants (intacs)
- Epikeratophakia / Epikeratoplasty

