What is Diabetic Retinopathy ?
Diabetes and the Eye
An increasing incidence of diabetes mellitus poses a major health problem in India. The contributing factors are:
- An inappropriate diet, high intake of fat and carbohydrates
- Sedentary lifestyle
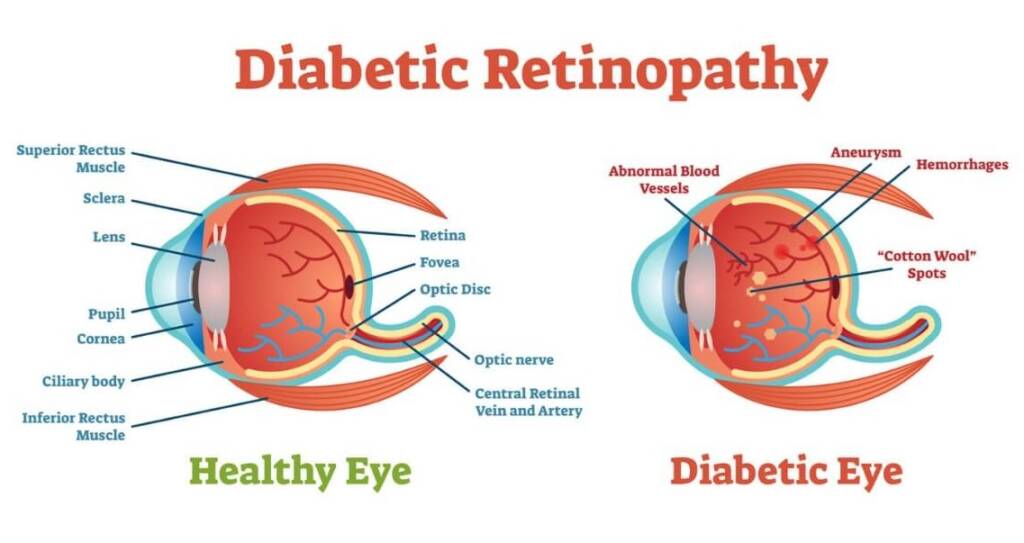
Diabetes may affect both the young (type I) and the old (type II). The latter type is far more common. Regardless of the type of diabetes, many diabetics develop a complication called diabetic retinopathy, a change in the retinal blood vessels that leads to loss of vision.
How does diabetes affect the eye?
Diabetes causes weakening of the blood vessels in the body. The tiny, delicate retinal blood vessels are particularly susceptible. This deterioration of retinal blood vessels, accompanied by structural changes in the retina, is termed diabetic retinopathy and will lead to loss of vision.
Diabetic retinopathy is gradual in onset and is related to the duration of diabetes. High blood glucose levels, high blood pressure and genetics influence the development and progression of diabetic retinopathy.
There are two main stages of diabetic retinopathy:
Non-proliferative: When the blood vessels leak, macular edema may occur, thereby reducing vision.
Proliferative: When new, weak blood vessels grow or proliferate, bleeding into the vitreous may occur and cause severe visual loss.
Diagnosis:
Diagnostic tools such as a slit lamp, ultrasound and procedures such as fluorescein angiography are used in addition to an ophthalmoscope to assess whether the patient has diabetic retinopathy or other eye problems.
Fluorescein Angiography:
This is a magnified photography of the retina using an injectable dye. It helps classify the condition, record changes in the retinal blood vessels, decide on the mode of treatment and evaluate the treatment.
Treatment:
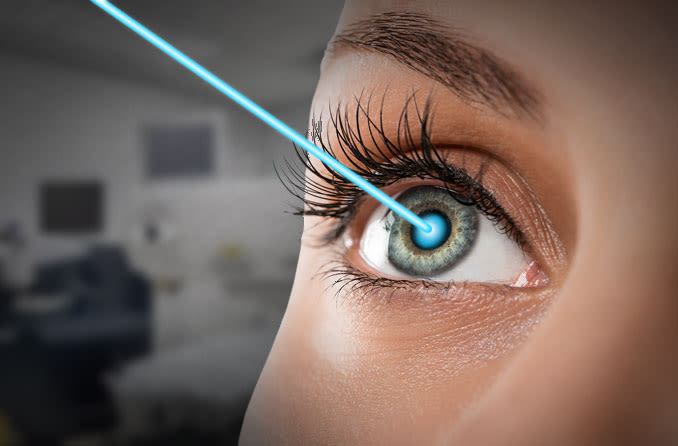
Lasers are widely used in treating diabetic retinopathy. Lasers are formed by an intense and highly energetic beam of light. They can slow down or stop the progression of diabetic retinopathy and stabilize vision.
Laser and it's side effects
Laser treatment is usually performed as an outpatient procedure. The patient is given topical anaesthesia to prevent any discomfort and is then positioned before a slit lamp.
The ophthalmologist directs the laser beam precisely on the target with the aid of the slit lamp and a special contact lens. Absorption by the diseased tissue either seals or destroys the tissue. Additional treatment may be required according to the patient’s condition.
Some patients may experience side effects after laser treatment. These are usually temporary. Possible side effects include watering of eyes, mild headache, double vision, glare or blurred vision. In the event of sudden pain or visual loss, the ophthalmologist must be contacted immediately.
What is Vitrectomy?
The retina is the light-sensing tissue at the back of the eye. The vitreous is the clear, jellylike substance that fills the middle of the eye. In some patients, there may be bleeding into the vitreous or the vitreous may pull the retina, reducing vision severely. In such instances the Vitreous is removed during vitrectomy surgery and usually replaced by saline solution.
The operation removes any blood or debris (from infection or inflammation) that may be blocking or blurring light as it focuses on the retina. Vitrectomy surgery removes scar tissue that can displace, wrinkle, or tear the retina. Vision is poor if the retina is not in its normal position. This surgery can also remove a foreign object stuck inside the eye as a result of injury.
Age Related Macular Degeneration (ARMD)
What is macular degeneration?
Macula is the most sensitive part of the retina, responsible for giving clear vision. Due to aging it can get degenerated. It is commonly referred to as age-related macular degeneration, and is often abbreviated as AMD. Age related macular degeneration is the most common cause of legal blindness in the geriatric population in the west and is probably more common in India than believed.
Dry ARMD causes thinning and atrophy of the macula with variable visual loss but is not amenable to any treatments as of now. Wet ARMD results from leakage or bleeding from choroidal neo vascularization and if untreated could lead to scarring and progressive visual loss. Conventional laser therapy has been found to be effective in the management of only a selected group of patients.
Treatment
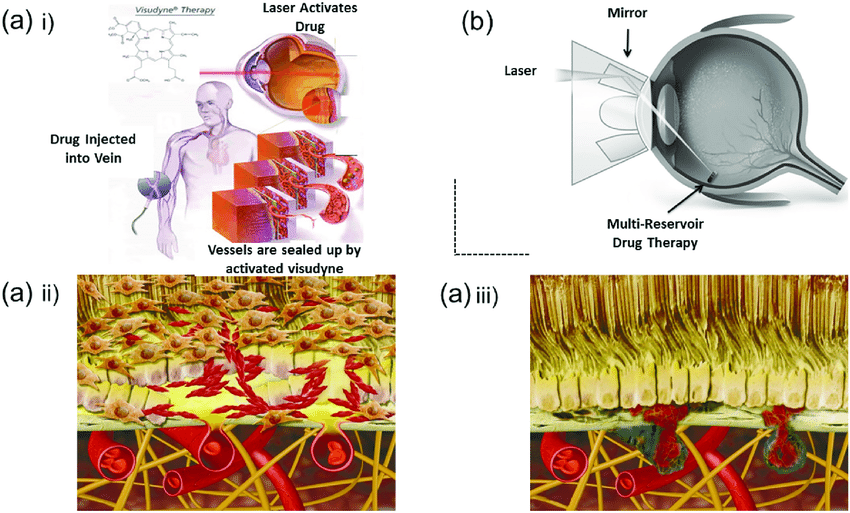
Photodynamic therapy (PDT) with Visudyne
The light sensitive drug, visudyne, is injected into the patient’s bloodstream which accumulates in the abnormal new vessels in the eye. This drug is activated by a nonthermal laser which closes the abnormal vessels without damaging the overlying sensory retina. Studies have shown that PDT slows the progression and improves vision in some forms of the disease.
Transpupillary Thermotherapy (TTT)
TTT is a cost effective alternative in the disease forms not eligible for PDT. This is a low energy diode laser which directly closes the abnormal vessels with a small risk of damage to the overlying retina.
Diabetic Retinopathy: A silent presence
- Diabetics are twice as likely as non-diabetics to develop eye problems. The most common eye complication in diabetes is diabetic retinopathy; other complications are cataract and glaucoma.
- Fifty percent of diabetics develop some degree of diabetic eye disease.
- The risk of blindness is 25 times higher in diabetics than in non-diabetics.
- Early detection and timely treatment of diabetic eye disease significantly reduces the risk of visual loss.
- Diabetic retinopathy is often symptomless in the early stages. Since only an ophthalmologist can detect early signs of diabetic retinopathy, all diabetics should have their eyes examined at least once every year.
Refractive Errors
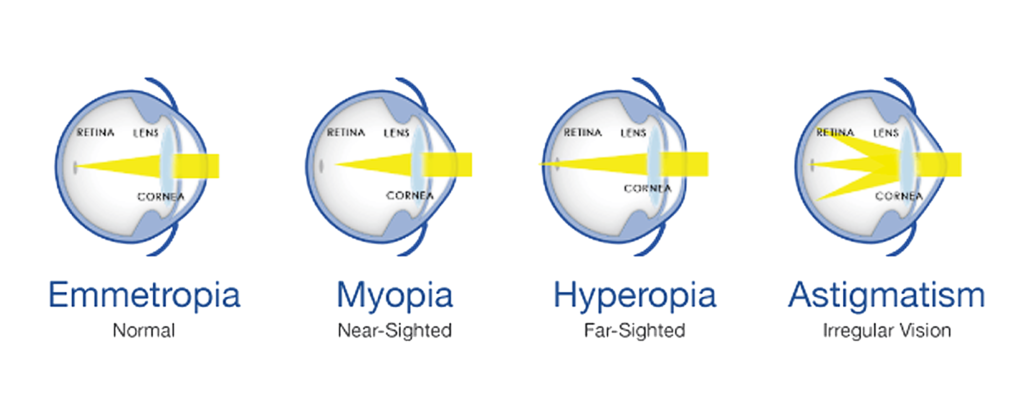
In normal vision, light rays from an object focus on the retina (emmetropia).
Alternatively, in the presence of refractive error, the light rays get focused in front or behind the retina causing blurred vision. Under normal conditions, as the eye ball grows in size from infancy to adulthood, there will be a corresponding change in curvature of cornea and the lens, enabling the eye to remain emmetropic, at all ages.
When one of these happens, refractive error occurs:
-
The eye ball being larger or smaller than the normal size
-
The corneal curvature being flatter or steeper than usual
-
Increase or decrease in the power of the lens
Symptoms of Refractive Errors
-
Children can have difficulty in reading small letters on the blackboard.
-
Some children squeeze their eyes while trying to see distant objects like blackboard, television etc.
-
Children hold books close to their face while reading.
-
Children with myopia have defective vision for distance and clear vision for near.
-
They can experience eye strain while trying to read for long hours.
-
Some children with hyperopia can present with squint.
-
Children can develop swellings on the lids due to constant rubbing of the eyes to see things clearly.
-
Eye pain and headache may occur.
The child should be checked by an ophthalmologist, if any one of the above symptoms is observed. The refractive errors can be classified as myopia (near sightedness) and hyperopia (far sightedness).
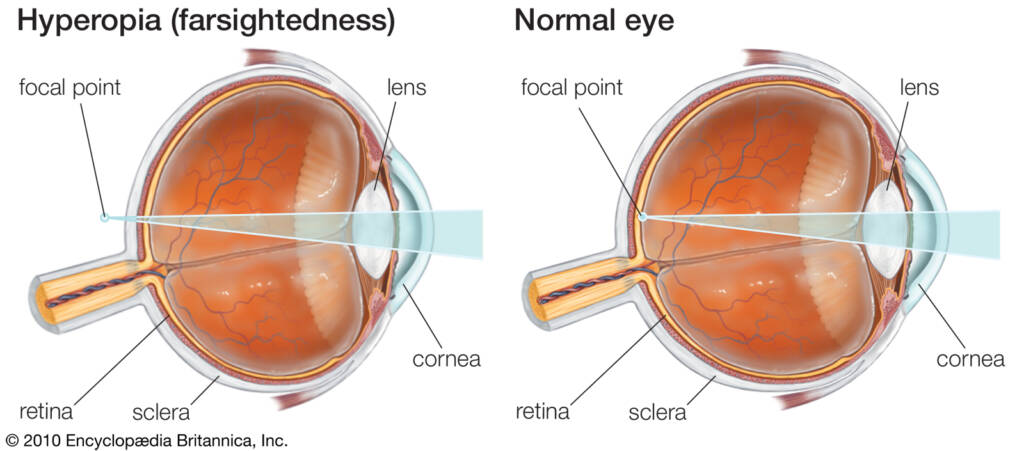
What is hyperopia?
In hyperopia or far sightedness, the light rays from an object form an image behind the retina.
Children with hyperopia
- Find difficulty in reading, writing and looking at both near and distant objects.
- Face eye strain while trying to read for long hours
- May have squint (crossed eyes)
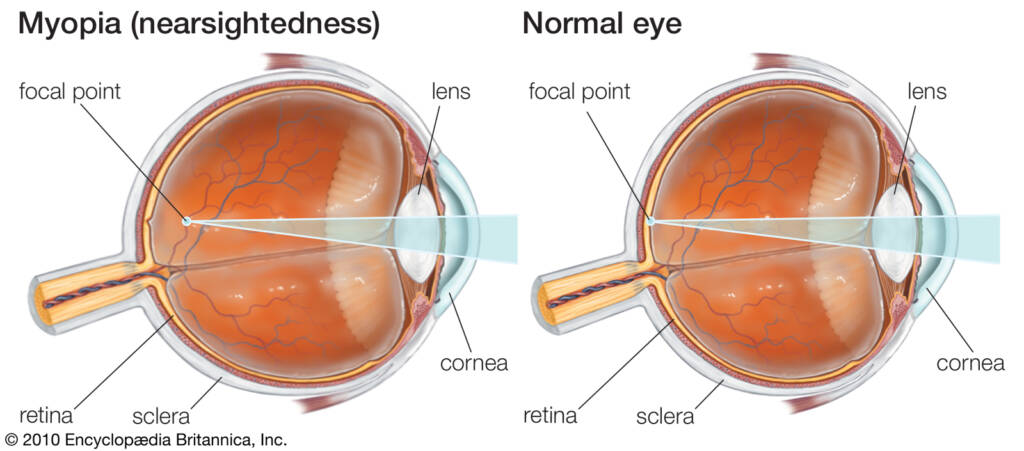
What is myopia?
In myopia or near sightedness, the light rays from an object form an image in front of the
retina.
Children with myopia
- Have defective vision for distance and clear vision for near
- Squeeze their eyes while trying to see distant objects
- Hold books close to their face while reading Children with the above conditions may also
- Rub their eyes constantly or blink frequently, because of the eye strain which they experience all the time or have pain, watering or burning sensation in the eyes
- Have headache in the forehead region which gets intensified in the evening
- Have recurrent swellings in the eye lids
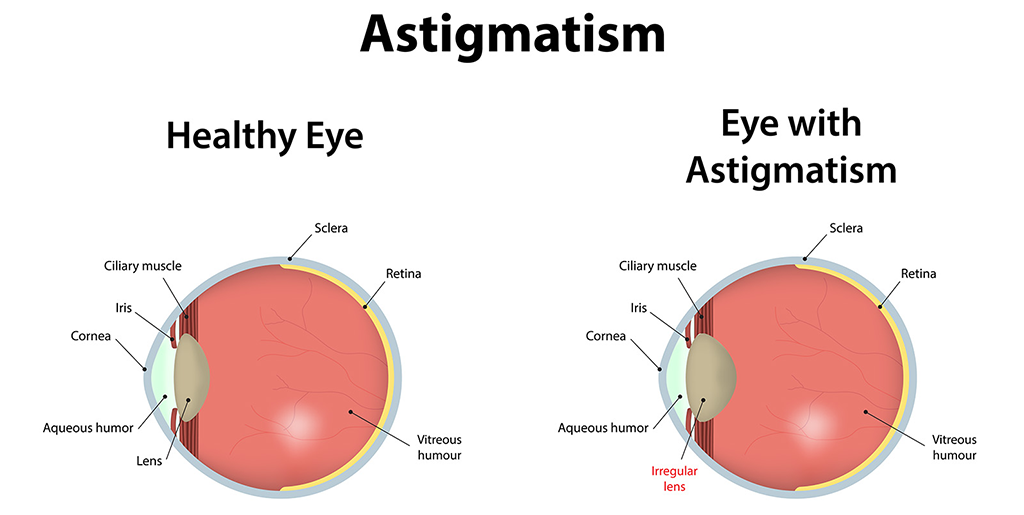
Astigmatism
This occurs due to changes in corneal curvature.
Treatment for the above conditions
- Correction using spectacles is the best option available. Though children may initially refuse to accept glasses, they will become fond of them once they realize
they can see better with them on. - The power of the glasses may change depending on the growth of the eye ball. An eye check-up and change of glasses if necessary, has to be done once in 6 months for children under 5 years of age and once a year thereafter. Making a child wear glasses regularly is the duty and responsibility of the parents.
- Failure to wear glasses in childhood when needed will retard the development of vision in that eye.
- Children older than 15 years can use contact lenses if they don’t want spectacles.
- Those over 18 to 20 years of age with stable power also have the option of
LASIK, a laser refractive surgery apart from contact lenses.
Failure to correct the refractive errors and the eventual low vision may hamper the academic activities of the child. So an ophthalmic consultation is essential in children, especially with symptoms of refractive errors. Finally, there is no relationship between nutritional deficiency and the occurrence of refractive error. So loading these children with Vitamin A will not help them. Sometime this may lead on to other complications.
LASIK - Refractive Surgery
LASIK ( Laser Insitu Keratomileusis ) is the high-tech out patient surgical technique for the treatment of myopia, astigmatism and hypermetropia. Utilising the accuracy and precision of the computer controlled excimer laser, LASIK changes the shape of the cornea and corrects refractive errors.
The MEL 80 from Zeiss (Germany) uses advanced software technology to perform LASIK. The procedure is relatively simple, painless and comfortable.
Remember
- Failure to correct refractive error leads to decreased vision and also hampers the academic activities of the child.
- Children found with symptoms of refractive errors should be brought to an ophthalmologist for necessary correction.
- Parents should encourage their children to wear glasses. Wearing glasses is not a stigma.
- Loading children with vitamin A may neither help in preventing nor correcting refractive errors.
- Spectacles themselves do not increase or decrease the power of the eye.
AMBLYOPIA - What is amblyopia?
Amblyopia is reduced vision in an anatomically normal eye. The term “lazy eye” is used to describe it.
When does amblypia develop?
Amblyopia develops when any of the following conditions occur:
Squint/Strabismus (eyes not positioned straight)
- There is a difference in power between the two eyes (one eye focuses differently from the other)
- Cataract (clouding of the lens)
- High or moderate power in both eyes
- Severe ptosis (droopy eyelids)
Children under 9 years of age whose vision is still developing are at the highest risk for amblyopia. Generally, the younger the child is, greater is the risk.
Why does amblyopia develop?
Amblyopia develops because when one eye is turned, as in squint, two different pictures are sent to the brain. In a young child, the brain learns to ignore the image of the deviated eye and see only the image of the better eye. Similarly when there is difference in power between the two eyes, the blurred image formed by the eye with greater power is avoided by the brain. In order that the retina may capture an object, it needs adequate light and visual stimulus. When these factors are absent, as in the presence of cataract, amblyopia results. A moderate or high degree of refractive power present in both eyes, when not
corrected early and adequately, also results in amblyopia.
What should be done?
Amblyopia can often be reversed if it is detected and treated early. Cooperation of the patient and parents is required to achieve good results. If left untreated or if not treated properly, the reduced vision or amblyopia becomes permanent and vision cannot be improved by any means.
How is amblyopia treated?
The most effective way of treating amblyopia is to make the child use the amblyopic eye. Covering or patching the good eye to force the use of the amblyopic eye may be necessary to ensure equal and normal vision. This can be achieved by:
- prescribing proper spectacles if the patient is found to have refractive error
- removal of cataract when indicated
- occluding the normal eye
- surgery, when amblyopia is accompanied by strabismus
Occlusion refers to closure of the normal eye with a patch, thus forcing the child to use the amblyopic eye. Occlusion is done from a few hours to a few days, depending upon the age of patient and the type and severity of amblyopia. In cases experiencing less severe amblyopia, partial occlusion, such as that by making one glass translucent, may be sufficient. Older children can do reading exercises at home while patching the normal eye. Those patients who are patching their eyes need periodic follow-up, which is scheduled with an ophthalmologist. Duration of treatment may extend from months to years. The ophthalmologist will decide for how long the occlusion should be continued. Loss of vision from amblyopia is preventable if treatment is begun early.
Facts on Patching
- Patching is not a pleasant thing for a child, so initially the child will be reluctant to undergo it. It is our duty to make the child understand the necessity of the procedure so that he/she will cooperate.
- In a young child patching is done for shorter periods initially; the duration is increased gradually to obtain better compliance.
- Acceptance is good as soon as vision improves in ambloypic eye.
Method of patching should be according to the interests of the child
- Patch should be stuck directly on the face over the eye.
- If the child wears glasses, the patch should be placed on the face, not on the glasses.
- Glasses can also be used as an occluder only in older children.
- Many children try to take the patch off. This problem usually disappears as the child grows accustomed to wearing the patch.
- Older children can be encouraged to read and young children can be involved in playing interesting games during patching.
- Precautions must be taken to prevent the child from peaking around the edge of the patch.
- Patching schedules should be followed strictly.
- Patching should not be stopped abruptly. The programme should be tapered only by ophthalmologists.
- Regular follow-up visits are a must.

