What is Retinopathy of Prematurity?
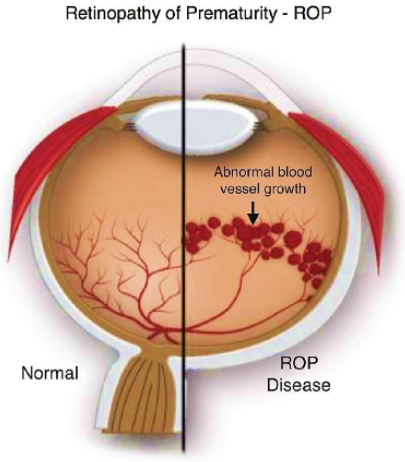
During development, blood vessels grow from the central part of the retina outwards. This process is completed few weeks before the normal time of delivery. The inside of the eye, the retina is not fully developed in premature babies. Retinopathy of Prematurity (ROP) occurs due to abnormal growth of blood vessels in an infant’s eye. If blood vessels grow normally, ROP does not occur. However, if the vessels grow and branch abnormally the baby develops ROP. These abnormal blood vessels can cause internal bleeding and even retinal detachment. This condition results in low vision or blindness – both of which are irreversible.
The incidence of ROP in India is between 38-51.9% and is as high as 80-100% in infants being less than 900 grams at birth or with gestational age less than 25 weeks. With the improved neonatal care, the incidence of ROP has increased. This is further compounded by the fact that the awareness of the condition is poor and lack of effective screening strategy.
How is ROP diagnosed?
The diagnosis of ROP is based on an effective screening strategy with good coordination between the NICU, neonatologist and the ophthalmologist (vitreo-retinal surgeon).
Whom to screen?
Infants with Birth weight < 2000 gms (Or)
Gestational Age at/ <36 weeks (Or)
Any premature baby with severe illness in perinatal period (RDS, sepsis, blood transfusion, IVH, apnoiec episodes, etc…).
When to screen?
At Anjani Eye Hospital we follow the ‘30 day’ strategy (i.e. the retinal examination should be completed at or before ‘day-30’ of life). Screening should preferably be done earlier (at 2 – 3 weeks of birth) in very low weight babies (<1200 gms) or in babies with very low gestational age (<28 weeks).

How to screen?
Screening for ROP is done by an ophthalmologist (vitreo-retinal surgeon) after dilatation of the pupil. After instillation of the topical anaesthetic eye drops, an infant lid speculum is placed and the examination of the eye performed. The examining doctor quickly does a general examination of the baby’s eyes followed by examination of the entire retina with the help of an indirect ophthalmoscopy.
The findings of the retina are duly noted by the examining doctor and the stage of the ROP mentioned.
How is ROP treated?
Not all eyes with ROP require treatment. However, in those eyes needing treatment, it is in the form of lasers, intra-vitreal anti-VEGF injections or surgery to reduce the chances of unfavourable disease outcomes.
Mild forms of ROP may resolve on their own without any active intervention. Severe forms of the disease on the other hand may need medical treatment as long as it is limited to stage 3. Surgical intervention is necessary once the disease reaches stage 4 or 5. The treatment helps stop further growth of abnormal vessels thus preventing vision loss.
If treated in time, the child is expected to have reasonably good vision. All premature babies need regular eye examinations till they start going to school.
They may need glasses or treatment for lazy eyes/ cross-eyes and sometimes, for cataract, glaucoma and retinal detachment.

Follow Up:
Once treated, life-long follow-up is needed for babies with ROP. All other premature infants irrespective of having ROP, a six monthly follow-up schedule should be maintained till the age of 5 years to rule out sequelae.
What are the complications of ROP?
Irrespective of treatment for ROP, these babies may have following complications:
- Refractive errors (most common)
- Squint
- Amblyopia (Lazy eye)
- Retinal Detachment
- Glaucoma
It is of utmost importance to refer premature babies to an ophthalmologist (vitreo-retinal surgeon) on time. Best way is, to follow the ‘30 day’ strategy. These examinations could save your patient’s sight and reduce the socioeconomic burden of such childhood blindness.
Frequently Asked Questions (FAQ)
Babies with a birth weight of less than 2000 grams or those born in under 35 weeks of pregnancy are most likely to have ROP.
Pre-term babies who have had problems after birth such as lack of Oxygen, infections, blood transfusions breathing trouble, etc., are also vulnerable.
Follow the “Day-30” strategy. The retinal examination should be completed before “day-30” of the life of a premature baby. It should preferably be done earlier (at 2-3 weeks of birth) in very low weight babies (<1200 grams birth weight).
ROP can progress in 7-14 days and therefore, needs a close follow-up till the retina matures.
ROP needs to be treated as soon as it reaches a critical stage called Threshold ROP. There is 50% or greater risk of vision loss if left untreated after this. Time is crucial.

